Afterinduction of Labor 3 Months Pregnant Again
- Enquiry
- Open Access
- Published:
Methods of consecration of labor and women's experience: a population-based accomplice study with mediation analyses
BMC Pregnancy and Childbirth book 21, Article number:621 (2021) Cite this article
Abstract
Background
Negative childbirth experience may affect mother wellbeing and health. However, information technology is rarely evaluated in studies comparing methods of induction of labor (IoL).
Aim
To compare women's feel of IoL co-ordinate to the method, considering the mediating role of interventions and complications of delivery.
Methods
We used data from the MEDIP prospective population-based cohort, including all women with IoL during 1 month in seven French perinatal networks. The experience of IoL, assessed at 2 months postpartum, was offset compared betwixt cervical ripening and oxytocin, and secondarily between dissimilar cervical ripening methods. Mediation analyses were used to measure the straight and indirect effects of cervical ripening on maternal experience, through delivery with interventions or complications.
Findings
The response rate was 47.8% (north = 1453/3042). Compared with oxytocin (north = 541), cervical ripening (n = 910) was associated less oft with feelings that labor went 'as expected' (adjusted risk ratio for the direct effect 0.78, 95%CI [0.70–0.88]), length of labor was 'acceptable' (0.76[0.71–0.82]), 'vaginal discomfort' was absent-minded (0.77[0.69–0.85]) and with lower global satisfaction (0.ninety[0.84–0.96]). Interventions and complications mediated betwixt 6 and 35% of the total effect of cervical ripening on maternal experience. Compared to the dinoprostone insert, maternal experience was not significantly unlike with the other prostaglandins. The balloon catheter was associated with less hurting.
Word
Cervical ripening was associated with a less positive experience of childbirth, whatever the method, merely partly explained by interventions and complications of delivery.
Determination
Counselling and support of women requiring cervical ripening might be enhanced to improve the experience of IoL.
Tweetable abstract
In the French electric current do, women's experience of induction of labor was less positive with cervical ripening, whatever the method, compared to oxytocin infusion: results of the MEDIP population-based accomplice of women with consecration of labor.
Statement of significance
Problem
Experience of induction of labor (IoL) is rarely assessed according to the method and results institute in RCT are not extrapolable in current exercise.
What is already known
Negative experience of IoL can take short- and long-term effects on female parent well-being and health and may be explained both by the methods and the outcomes of IoL.
What this newspaper adds
Using population-based data, feel of Iol was less positive with cervical ripening. Feel of IoL was non different co-ordinate to the ripening method and was but partly explained by the interventions and complications.
Introduction
Women'south experience and satisfaction with childbirth is an important chemical element for judging the quality of care in a maternity ward [ane]. From 5 to 20% of women describe their experience of delivery as negative [2,3,4]. These negative experiences may have short- and long-term effects: harm of the mother-kid bail from the very start, postpartum depression, decisions to non become pregnant once more, fear of commitment, and requests for a repeat cesarean for a subsequent pregnancy [5,6,7,8,9]. Mostly, patients' experience in hospitals is best when the medical outcomes of an intervention are both adept and uncomplicated [10]. Women's feel in childbirth is known to be worse when they accept a cesarean delivery, especially when it is performed equally an emergency [xi, 12].
Ane of the most mutual interventions in obstetrics today is induction of labor (IoL). In most developed countries, one woman in v has labor induced [13,14,15]. The selection of the method depends in part on the clinical exam of cervical ripeness. Intravenous oxytocin infusion and amniotomy are recommended when the cervix is favorable, otherwise cervical ripening is necessary to increase the likelihood of successful induction [sixteen]. Several methods of cervical ripening are unremarkably used because the data currently available do not justify to recommend one method over whatsoever other [17,eighteen,xix,20,21,22].
Most studies comparing methods of IoL accept assessed their effectiveness and safety. Following a Delphi process, Dos Santos et al. [23] listed maternal experience of childbirth and satisfaction in the set of core outcomes that should routinely been assessed in studies dealing with IoL. A review of the literature has shown that only around five% of the trials of consecration report women'due south experience of it [24]. The extrapolation of the results of trials is questionable considering the populations included are highly selected and the women receive both standardized management and special attention because of their participation in the trial [25]. To our knowledge, no observational report has assessed women'south experience according to the method of induction in routine care with population-based data.
The objective of this study was to compare, in a population-based cohort of women who underwent consecration of labor, the experience of delivery according to the method used, taking into account the mediating contribution of intervention and complication of delivery.
Material and methods
This was a comparative written report using the data of the MEDIP (Methods of consecration of labor and perinatal outcomes) prospective population-based cohort. The objective of the MEDIP study was to depict the practices of induction in France and to compare the effectiveness and safety of the different methods in current use [19]. This cess of women'southward experience was one of the planned secondary objectives of the study.
The cohort included all women who had labor induced from 17 November to 21 December 2015 in all maternity units belonging to 7 perinatal health networks (n = 94). These units deemed for 1-sixth of the annual deliveries in France and were representative of the unabridged set of French maternity units [26]. Still nascence and medically-indicated termination of pregnancy were exclusion criteria. A follow-up of 2-months was performed.
Data were recorded prospectively. The midwife or obstetrician managing the woman informed the indication of IoL, the method used and the Bishop score at the onset of induction. The pick of method was based on each maternity ward's habits or was left to the practitioner's choice. Contained clinical research technicians recorded boosted data from the adult female'southward medical records. Experience of induction was assessed with a self-administered questionnaire sent by post or e-mail (three reminders) at 2 months postpartum.
The experience of IoL was first compared between women who underwent cervical ripening as start method of IoL and those who did non, i.e. those who received oxytocin infusion every bit start method (exposure/outcomes associations A). Secondarily, the experience of commitment was compared according to each method of cervical ripening (exposure/outcomes associations B). We compared the methods mainly used in the MEDIP cohort: vaginal dinoprostone pessary equally a dull-release insert (as reference, considering it was the method used most frequently), dinoprostone as a vaginal gel, misoprostol as a vaginal tablet and an intracervical balloon (Cook® balloon or Foley catheter). We excluded women who received PGE2 intracervical gel (due north = 3) or intravenous PGE2 (n = 7) or membranes sweeping only (n = one) because the number of women was besides minor to perform statistical comparisons for these methods (Fig. 1). In the MEDIP study, all methods of labor induction were used individually, with no combination of two methods simultaneously. Specific modes of usage of the methods in this accomplice take previously been described [27].
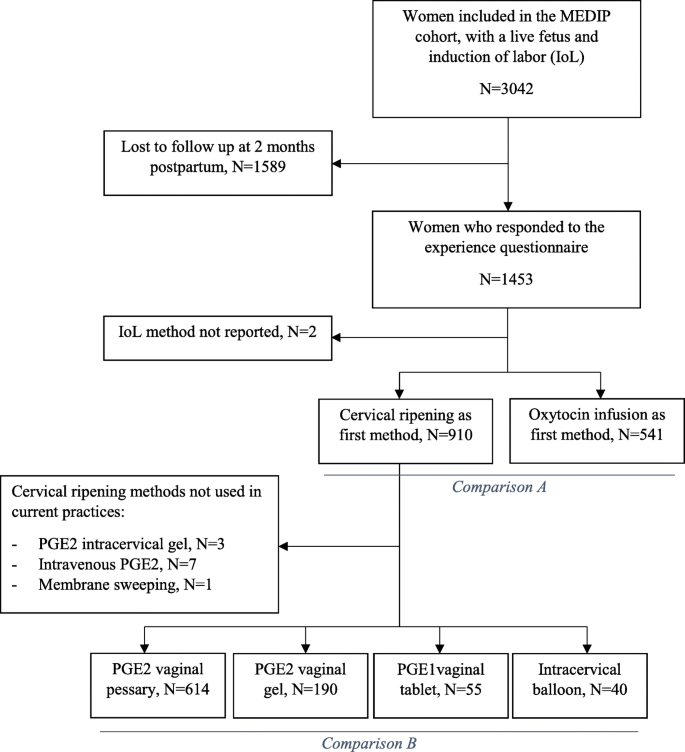
Flowchart of study population. Legend: Iol, induction of labor; PG, prostaglandins
For assessing women's feel, a specific questionnaire was adult after a review of qualitative research on the topic past the report Scientific Committee, a multidisciplinary group of perinatal professionals, epidemiologists and user representatives [28,29,30]. We analysed eight cocky-administered questions about the grade of labor and delivery, vaginal discomfort, maximum pain, global satisfaction and the likelihood that woman would choose the same method of induction again. Some categories were regrouped to obtain binary outcomes to study positive experience of childbirth (Boosted file 1).
A directed acyclic graph (http://www.dagitty.internet/) presented the assumed exposure-outcome pathway with misreckoning and mediators variables (Additional file 2). We considered that the outcomes of consecration were mediators in the causal pathway betwixt the consecration method used and the feel of consecration. For this reason, we did non adapt for these variables [31]. To accept them into business relationship, the outcomes of IoL were integrated as mediators. Mediation analysis decompose the total consequence of the causal pathway betwixt an exposure and an result into a direct and an indirect issue. The indirect effect estimated is the extent to which the method of labor induction affects women'south experience through the outcomes of commitment. The outcomes of induction were summarized in a blended variable called 'commitment with intervention or complication', that is, whatever combination of a cesarean or operative vaginal delivery, postpartum hemorrhage (full estimated claret loss ≥500 ml), severe perineal laceration or NICU access. We adjusted for parity and history of C-department, trunk mass alphabetize, peridural analgesia, maternal age, medical indication and maternity status. We also adjusted for Bishop score when measuring the association between the experience of commitment according to each method of cervical ripening (B) just not for the first comparisons (A). In fact, adjusting for Bishop score may lead to overfitting because it is strongly correlated with the choice of performing cervical ripening or not. Interaction for parity and medical indication of IoL was tested.
Statistical analyses
Multivariable Poisson regression models were performed to obtain take chances ratios. A robust variance was used to take the cluster consequence into business relationship. For the mediation assay, we used the inverse odds weighting (IOW) method described by Nguyen et al. [32, 33] IOW is a weight-based approach that condenses the clan between the exposure and the mediator into a weight. It is a stepwise procedure. Showtime, nosotros estimated for each woman the predictive odds of 'undergoing cervical ripening' due to a 'commitment with intervention or complications'. The inverse of this predicted odds gives a weight. Secondarily, the direct effect of cervical ripening on maternal experience was estimated past using weighted Poisson regression. Then, the indirect effect was calculated past subtracting the direct from the total effect coefficients. The proportion mediated (PM) was calculated as the ratio of the total effect to the indirect effect [34]. Confidence intervals for indirect effect and PMs were obtained by bootstrapping. Complete case analyses were performed because outcome data were missing for fewer than 2% of the women who responded to the questionnaire. The statistical analyses were performed with Stata/SE software, version 15.0.
Results
Of the 3042 women included in the MEDIP cohort, 1453 (47.8%) responded to the self-administered questionnaire at 2 months postpartum. (49% by mail and 51% by e-mail). The respondents included a higher proportion of women who were nulliparous, older than 35 years, born in Europe, living with a partner, who belonged to higher socio-professional categories and who did not receive intracervical balloon for IoL. The response was non associated with more than unfavorable outcomes or with medical interventions during commitment (Fig. 1).
Women's characteristics of respondents and experience co-ordinate to method of induction are described in Tabular array one and Table 2. Compared with women receiving oxytocin (n = 541), those who underwent cervical ripening (n = 910) had a less positive experience of induction. After taking the confounding and mediating factors into account, cervical ripening was significantly associated with a lower take a chance of experiencing that 'labor went quite normally' (RR adapted for direct effect, aRR 0.86, 95% CI 0.81–0.93), that 'labor and delivery went every bit expected' (direct aRR = 0.78, 95% CI 0.seventy–0.88 and aRR 0.88, 95% CI 0.79–0.98) and that the 'length of labor was adequate' (direct aRR 0.76, 95% 0.71–0.82). Cervical ripening was also associated with less 'absenteeism of sensation of vaginal discomfort' (direct aRR 0.77, 95% CI 0.69–0.85), maximum pain 'less than eight/10' (straight aRR 0.59, 95% CI 0.51–0.70), a poorer 'global satisfaction' (straight aRR 0.xc, 95% CI 0.84–0.96), and less willingness to have some other consecration 'by the aforementioned method' (direct aRR 0.83, 95% CI 0.78–0.88). Tests of interaction for parity and medical indication for induction of labor were non-significant. Between 6 and 35% of the association between cervical ripening and experience was significantly mediated past the variable 'delivery with intervention or complications' (Tabular array 3).
Comparing the dinoprostone insert (reference) to the other types of prostaglandins, the experience of IoL did not differ significantly for virtually items, except that more women who received the intravaginal misoprostol tablet did not experience vaginal discomfort (straight aRR 1.34, 95% 1.20–1.48) (Tabular array 4). The intracervical balloon was associated with more frequent rating of maximum hurting lower than 8/10 (directly aRR 1.78, 95% CI 1.twenty–2.65).
Give-and-take
Principal findings
Experience of consecration of labor was less positive for women requiring cervical ripening. Women deplored a greater gap between what was expected and what was experienced, more unacceptable duration of labor, vaginal discomfort, intense pain, and insatisfaction with induction. Most of the experience was explained past the method and not past the interventions or complications of commitment. The women'south experience did not seem different between the prostaglandins but ripening with the balloon catheter seemed associated with less intense pain.
Strengths and limitations
This is to our knowledge the first study to examine specifically multiple domains of the experience of IoL associated with cervical ripening with population-based information while taking into account the mediating role of interventions and complications. The MEDIP study was specifically designed to study perinatal outcomes associated with the unlike methods of consecration of labor in France [19, 26]. The prospective data drove about the class of induction ensured the quality of the information reported.
Our report had some limits. A non-validated questionnaire was used, considering the existing scales did not appear advisable for a specific evaluation of the experience of IoL. Since the MEDIP report was performed, the Get out scale (Feel of induction tool) has been developed in Australia for this purpose, but it has never been validated in another population [35]. External validity is as well questionable considering the women included came from perinatal networks not randomly selected, although characteristics of maternity units participating in this big sample were comparable to those of all French maternity units [26]. In that location was also a selection bias of respondent women who were nearly frequently European and employed. This questionnaire was sent at 2 months because memories of facts immediately later on delivery may be modified, due to tiredness or lack of time to integrate the course of events. Moreover, interviewing women during their stay in the maternity unit of measurement may accept led the woman interviewed to provide data that she felt comfortable with the intendance providers. We cannot know whether the responses were biased toward women with less or worse positive feel or not. Nonetheless, we showed that the response was non associated with interventions or complications. Finally, a stiff proportion of the feel was probably afflicted past the environment of birth, the specific organization of a maternity ward or the individual relation created between the woman and the provider supporting and caring for her [36, 37]. Such information might have been particularly relevant for comparison of dissimilar cervical ripening methods, for which the usage are heterogeneous and depend on maternity unit's preferences [26].
Estimation
These information about how women experience IoL co-ordinate to the method used might exist relevant for guiding the management of intendance. Qualitative studies have already shown that a negative feel of induction was associated with a lack of training and information most the benefits and risks of induction and its grade, to the intensity of pain, the elapsing of the induction and to a poorer medical result, in particular, emergency cesarean delivery [36, 37]. These studies didn't distinguished specifically women with cervical ripening. When comparing woman satisfaction between oxytocin alone and vaginal prostaglandins E2, a meta-assay of Alfirevic et al. [16] previously found no departure. However, the three trials included had a different fashion of measuring maternal satisfaction and the studies were probably not representative of bodily obstetric exercise.
The less positive experience of childbirth with cervical ripening does not imply that oxytocin should be proposed whatever the degree of cervix immaturity. Indeed, cervical ripening is recommended in example of unfavourable cervix [38, 39]. However, it calls for stronger support and counselling. In France, most pregnant women attend antenatal birth classes, especially the nulliparous women, but the content of these classes are probably very heterogeneous. Antenatal education on what to expect afterward induction on labor co-ordinate to the method should probably exist enhanced [xiii]. Moreover, one-to-one support for management of pain, which is not usual in French practices would certainly be skilful for improving maternal experience [37].
Our results also raise questions, equally the number of constituent IoL might be increased in the coming years. Indeed, recent data have demonstrated meliorate perinatal outcomes with elective induction of labor at term, regardless of cervical status [40,41,42]. In the Make it trial comparing consecration of labor with expectant management among 6000 low-risk nulliparous women at 39 weeks of gestation, induction of labor resulted in a better global experience and less pain [43]. Results were not stratified co-ordinate to the method of induction. I limitation is that the experience of women who agreed to participate to such trial may not exist representative of that of women in full general population. They volunteered to participate and may have been more inclined to experience their induction positively whatsoever the method used. In the review of observational written report comparing consecration of labor with expectant direction, women's feel was not evaluated [42]. Our results tin can non imply that women who had unfavourable cervix expectantly managed instead of existence induced would have had a better experience. All the same, in the absenteeism of a medical indication, waiting for the neck to be more favourable may be an alternative to improve maternal experience.
The few studies comparison the experience of different methods of cervical ripening also found greater discomfort and stronger pain during induction by prostaglandins compared with the airship, but overall global satisfaction did not differ [44, 45]. This may be explained by the fact that the balloon appears to have a mechanical ripening activeness but not contraction-inducing effect that may be less painful. These results merit further exploration in view of the modest number of women induced with the balloon included in these studies as in our report.
Conclusion
In current do, cervical ripening was associated with a less positive experience of Iol, the major part of information technology was non explained by the interventions and complications of delivery. Counselling and support of women requiring cervical ripening might better the feel of induction of labor. Further data about experience according to the method of cervical ripening are necessary.
Availability of information and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Iol:
-
Induction of labor
- BMI:
-
Body mass alphabetize
- CS:
-
Cesarean section;
- PPH:
-
Postpartum hemorrhage
- NICU:
-
Neonatal intensive intendance unit
- RCT:
-
Randomized controlled trial
References
-
Goberna-Tricas J, Banús-Giménez MR, Palacio-Tauste A, Linares-Sancho S. Satisfaction with pregnancy and birth services: the quality of maternity care services equally experienced by women. Midwifery. 2011;27(6):e231–7. https://doi.org/10.1016/j.midw.2010.10.004.
-
Henriksen L, Grimsrud Eastward, Schei B, Lukasse K, Bidens study group. Factors related to a negative nascence experience - a mixed methods study. Midwifery. 2017;51:33–9. https://doi.org/10.1016/j.midw.2017.05.004.
-
Smarandache A, Kim THM, Bohr Y, Tamim H. Predictors of a negative labour and birth experience based on a national survey of Canadian women. BMC Pregnancy Childbirth. 2016;16(1):114. https://doi.org/x.1186/s12884-016-0903-2.
-
Waldenström U, Rudman A, Hildingsson I. Intrapartum and postpartum care in Sweden: women'due south opinions and risk factors for non being satisfied. Acta Obstet Gynecol Scand. 2006;85(5):551–60. https://doi.org/10.1080/00016340500345378.
-
Gottvall K, Waldenström U. Does a traumatic birth experience have an impact on hereafter reproduction? BJOG Int J Obstet Gynaecol. 2002;109(3):254–lx. https://doi.org/ten.1111/j.1471-0528.2002.01200.10.
-
Størksen HT, Garthus-Niegel S, Vangen S, Eberhard-Gran M. The impact of previous nascence experiences on maternal fear of childbirth. Acta Obstet Gynecol Scand. 2013;92(three):318–24. https://doi.org/10.1111/aogs.12072.
-
Bell AF, Rubin LH, Davis JM, Golding J, Adejumo OA, Carter CS. The birth experience and subsequent maternal caregiving attitudes and behavior: a birth cohort study. Curvation Womens Ment Health. 2019;22(5):613–20. https://doi.org/10.1007/s00737-018-0921-3.
-
Bong AF, Andersson E. The birth experience and women's postnatal depression: a systematic review. Midwifery. 2016;39:112–23. https://doi.org/10.1016/j.midw.2016.04.014.
-
Hildingsson I, Rådestad I, Rubertsson C, Waldenström U. Few women wish to be delivered by caesarean section. BJOG Int J Obstet Gynaecol. 2002;109(6):618–23. https://doi.org/ten.1111/j.1471-0528.2002.01393.x.
-
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open up. 2013;iii(1):e001570. https://doi.org/ten.1136/bmjopen-2012-001570.
-
Handelzalts JE, Waldman Peyser A, Krissi H, Levy South, Wiznitzer A, Peled Y. Indications for emergency intervention, mode of delivery, and the childbirth experience. PLoS One. 2017;12(1):e0169132. https://doi.org/10.1371/journal.pone.0169132.
-
Carquillat P, Boulvain M, Guittier M-J. How does delivery method influence factors that contribute to women'southward childbirth experiences? Midwifery. 2016;43:21–8. https://doi.org/10.1016/j.midw.2016.10.002.
-
Blondel B, Coulm B, Bonnet C, Goffinet F, le Ray C, National Coordination Grouping of the National Perinatal Surveys. Trends in perinatal health in metropolitan French republic from 1995 to 2016: results from the French National Perinatal Surveys. J Gynecol Obstet Hum Reprod. 2017;46(10):701–13. https://doi.org/10.1016/j.jogoh.2017.09.002.
-
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Mathews TJ. Births: last data for 2015. Natl Vital Stat Rep Cent Dis Command Prev Natl Cent Health Stat Natl Vital Stat Syst. 2017;66(1).
-
European Perinatal Wellness Report 2010 - Euro-Peristat. https://world wide web.europeristat.com/reports/european-perinatal-health-written report-2010.html.
-
Alfirevic Z, Kelly AJ, Dowswell T. Intravenous oxytocin solitary for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2009:CD003246. https://doi.org/10.1002/14651858.CD003246.pub2.
-
Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Dias S, Jones LV, et al. Labour induction with prostaglandins: a systematic review and network meta-analysis. BMJ. 2015;350(feb05 10):h217. https://doi.org/x.1136/bmj.h217.
-
Chen W, Xue J, Peprah MK, Wen SW, Walker M, Gao Y, et al. A systematic review and network meta-analysis comparing the apply of Foley catheters, misoprostol, and dinoprostone for cervical ripening in the consecration of labour. BJOG Int J Obstet Gynaecol. 2016;123(three):346–54. https://doi.org/x.1111/1471-0528.13456.
-
Blanc-Petitjean P, Carbonne B, Deneux-Tharaux C, Salomé G, Goffinet F, le Ray C, et al. Comparison of effectiveness and safety of cervical ripening methods for consecration of labour: a population-based study using coarsened exact matching. Paediatr Perinat Epidemiol. 2019;33(5):313–22. https://doi.org/10.1111/ppe.12569.
-
De Vivo Five, et al. Early on amniotomy after cervical ripening for consecration of labor: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2020;222(4):320–9. https://doi.org/10.1016/j.ajog.2019.07.049.
-
Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, Rex VJ, et al. Methods of induction of labour: a systematic review. BMC Pregnancy Childbirth. 2011;eleven(one):84. https://doi.org/10.1186/1471-2393-eleven-84.
-
Di Mascio D, et al. Maternal and neonatal outcomes of pregnancies complicated by late fetal growth brake undergoing induction of labor with dinoprostone compared with cervical balloon: a retrospective, international study. Acta Obstet Gynecol Scand. 2021;100(7):1313–21. https://doi.org/10.1111/aogs.14135.
-
Dos Santos F, Drymiotou South, Antequera Martin A, Mol BW, Gale C, Devane D, et al. Development of a cadre outcome ready for trials on induction of labour: an international multistakeholder Delphi study. BJOG Int J Obstet Gynaecol. 2018;125(xiii):1673–80. https://doi.org/x.1111/1471-0528.15397.
-
Medley Due north, et al. Outcomes reported in trials of methods for the induction of labour. Trials. 2015;16:P4 1745–6215-16-S1-P4.
-
Rothwell PM. External validity of randomised controlled trials: 'to whom exercise the results of this trial apply?'. Lancet Lond Engl. 2005;365(9453):82–93. https://doi.org/10.1016/S0140-6736(04)17670-8.
-
Blanc-Petitjean P, Salomé M, Dupont C, Crenn-Hebert C, Gaudineau A, Perrotte F, et al. Labour induction practices in France: a population-based declarative survey in 94 maternity units. J Gynecol Obstet Hum Reprod. 2018;47(ii):57–62. https://doi.org/10.1016/j.jogoh.2017.11.006.
-
Blanc-Petitjean P, et al. Overview of induction of labor practices in France. Gynecol Obstet Fertil Senol. 2019;47:555–61.
-
Jay A, Thomas H, Brooks F. In labor or in limbo? The experiences of women undergoing induction of labor in hospital: Findings of a qualitative written report. Birth Berkeley Calif. 2018;45:64–70.
-
Shetty A, Burt R, Rice P, Templeton A. Women'due south perceptions, expectations and satisfaction with induced labour--a questionnaire-based study. Eur J Obstet Gynecol Reprod Biol. 2005;123(1):56–61. https://doi.org/x.1016/j.ejogrb.2005.03.004.
-
Henderson J, Redshaw M. Women's experience of induction of labor: a mixed methods study. Acta Obstet Gynecol Scand. 2013;92(10):1159–67. https://doi.org/10.1111/aogs.12211.
-
Ananth CV, Schisterman EF. Confounding, causality, and confusion: the role of intermediate variables in interpreting observational studies in obstetrics. Am J Obstet Gynecol. 2017;217(2):167–75. https://doi.org/ten.1016/j.ajog.2017.04.016.
-
Nguyen QC, Osypuk TL, Schmidt NM, Glymour MM, Tchetgen Tchetgen EJ. Applied guidance for conducting mediation analysis with multiple mediators using inverse odds ratio weighting. Am J Epidemiol. 2015;181(5):349–56. https://doi.org/10.1093/aje/kwu278.
-
Tchetgen Tchetgen EJ. Inverse odds ratio-weighted estimation for causal arbitration assay. Stat Med. 2013;32(26):4567–80. https://doi.org/ten.1002/sim.5864.
-
Ananth CV. Proportion mediated in a causal arbitration analysis: how useful is this measure? BJOG Int J Obstet Gynaecol. 2019;126:983.
-
Beckmann 1000, Thompson R, Miller Y, Prosser SJ, Flenady Five, Kumar S. Measuring women's feel of induction of labor using prostaglandin vaginal gel. Eur J Obstet Gynecol Reprod Biol. 2017;210:189–95. https://doi.org/10.1016/j.ejogrb.2016.12.032.
-
Akuamoah-Boateng J, Spencer R. Woman-centered care: Women's experiences and perceptions of consecration of labor for uncomplicated post-term pregnancy: a systematic review of qualitative evidence. Midwifery. 2018;67:46–56. https://doi.org/10.1016/j.midw.2018.08.018.
-
Coates R, Cupples G, Scamell A, McCourt C. Women'due south experiences of induction of labour: qualitative systematic review and thematic synthesis. Midwifery. 2019;69:17–28. https://doi.org/ten.1016/j.midw.2018.x.013.
-
ACOG Exercise Bulletin No. 107. Induction of labor. Obstet Gynecol. 2009;114(386–397).
-
Induction of Labour. Imperial College of Obstetricians and Gynaecologists https://www.rcog.org.uk/en/guidelines-inquiry-services/guidelines/induction-of-labour/.
-
Bernardes TP, Broekhuijsen Grand, Koopmans CM, Boers KE, van Wyk L, Tajik P, et al. Caesarean department rates and agin neonatal outcomes after induction of labour versus expectant management in women with an unripe cervix: a secondary analysis of the HYPITAT and DIGITAT trials. BJOG Int J Obstet Gynaecol. 2016;123(9):1501–8. https://doi.org/ten.1111/1471-0528.14028.
-
Miller NR, Goose egg RL, Foglia LM, Pates JA, Nielsen PE. Elective induction of labor compared with expectant Direction of Nulliparous Women at 39 weeks of gestation: a randomized controlled trial. Obstet Gynecol. 2015;126(6):1258–64. https://doi.org/x.1097/AOG.0000000000001154.
-
Grobman WA, Caughey AB. Elective consecration of labor at 39 weeks compared with expectant direction: a meta-assay of cohort studies. Am J Obstet Gynecol. 2019;221(four):304–10. https://doi.org/10.1016/j.ajog.2019.02.046.
-
Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, et al. Labor induction versus expectant Management in low-Risk Nulliparous Women. N Engl J Med. 2018;379(half-dozen):513–23. https://doi.org/10.1056/NEJMoa1800566.
-
Pennell CE, Henderson JJ, O'Neill MJ, McCleery S, Doherty DA, Dickinson JE. Induction of labour in nulliparous women with an unfavourable cervix: a randomised controlled trial comparing double and unmarried balloon catheters and PGE2 gel. BJOG Int J Obstet Gynaecol. 2009;116(eleven):1443–52. https://doi.org/10.1111/j.1471-0528.2009.02279.10.
-
Henry A, Madan A, Reid R, Tracy SK, Austin Thou, Welsh A, et al. Outpatient Foley catheter versus inpatient prostaglandin E2 gel for induction of labour: a randomised trial. BMC Pregnancy Childbirth. 2013;13(one):25. https://doi.org/x.1186/1471-2393-13-25.
Acknowledgements
The MEDIP study was conducted by Assistance Public-Hôpitaux de Paris (Département de la recherche Clinique et du développement). The authors give thanks all the members of the MEDIP study scientific committee: Catherine Crenn-Hebert, Adrien Gaudineau, Frédérique Perrotte, Pierre Raynal, Elodie Clouqueur, Gaël Beucher, Catherine Deneux-Tharaux, Pierre-Yves Ancel, and all the local investigators for their contributions to the MEDIP study. The authors also give thanks the URC-CIC Paris Descartes Necker/Cochin (Laurence Lecomte, Isabelle Apr and Marina Salomé) for setting upward and monitoring the MEDIP study, all the women who agreed to participate in information technology and the midwives who recruited and included them.
Funding
Data comes from the MEDIP study, funded by the national agency for drug safety and health products (ANSM) as role of a call for research projects (No. AAP-2014-030). Pauline Blanc-Petitjean's PhD research was funded by a research grant by Help Publique-Hôpitaux de Paris.
Author information
Affiliations
Consortia
Contributions
CLR and FG conceived the study. PBP, CLR, CD, MS, BC and FG contributed to its design, conducted the analyses, performed the report, drafted the original manuscript, reviewed and revised the manuscript. All authors approved the final manuscript every bit submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The MEDIP protocol was registered in the ClinicalTrial database (22/06/2015, No. NCT02477085) and approved by the Patient Protection Commission of Ile de French republic i in May 2015 (CPPIDF1–2015-May-DAP 21bis). The CCTIRS (No.15.609) and the CNIL (MMS/VCS/AR1510301) authorized the use of the data for this study. Informed consent was obtained from all women included in the cohort. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
All authors have read and approved the content, and agree to submit the manuscript for consideration for publication in your journal.
Competing interests
The authors accept no competing interests or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Boosted information
Publisher's Notation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table.
Items of the self-administered questionnaire evaluating the positive feel of induction of labor.
Additional file ii: Figure.
Directed acyclic graph for the association betwixt the method of labor induction and maternal feel. Legend: DAG created with the web-based awarding DAGitty (http://www.dagitty.net/). CS: caesarean section, BMI: body mass index.
Additional file 3: Table.
Characteristics and major outcomes of women who did and did not respond to the questionnaire.
Rights and permissions
Open up Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as y'all give appropriate credit to the original author(due south) and the source, provide a link to the Artistic Eatables licence, and indicate if changes were fabricated. The images or other third party cloth in this commodity are included in the commodity's Artistic Commons licence, unless indicated otherwise in a credit line to the material. If textile is non included in the commodity's Artistic Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted employ, you will demand to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Eatables Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zilch/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
About this article
Cite this article
Blanc-Petitjean, P., Dupont, C., Carbonne, B. et al. Methods of induction of labor and women's experience: a population-based accomplice study with mediation analyses. BMC Pregnancy Childbirth 21, 621 (2021). https://doi.org/10.1186/s12884-021-04076-x
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12884-021-04076-ten
Keywords
- Induction of labor
- Cervical ripening
- Maternal feel, midwifery research, causal mediation assay
Source: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-04076-x